Paper Published in Science of The Total Environment
A team of scientists at University of Houston Department of Earth and Atmospheric Sciences examined air movement outdoors and its effects on the spread of respiratory diseases like COVID-19. The findings published online in Science of The Total Environment.
“While most studies have looked at how air circulates indoors, we wanted to explore the outdoor environment where ventilation is different,” said Hadi Zanganeh Kia, an atmospheric sciences Ph.D. student in the UH Air Quality Forecasting group led by Dr. Yunsoo Choi, associate professor of atmospheric science. “We simulated the movement of a sneeze in areas where the air doesn't circulate well, called ‘hot spots.’” Kia was the first author on the paper.
Others on the paper were Choi, Delaney Nelson, Jincheol Park, and Arman Pouyaei, all with UH EAS.
“This study is an important application using computational fluid dynamics modeling, and it highlights the importance of understanding the dynamics of outdoor air movement and its role in the spread of respiratory diseases, including COVID-19,” Choi said.
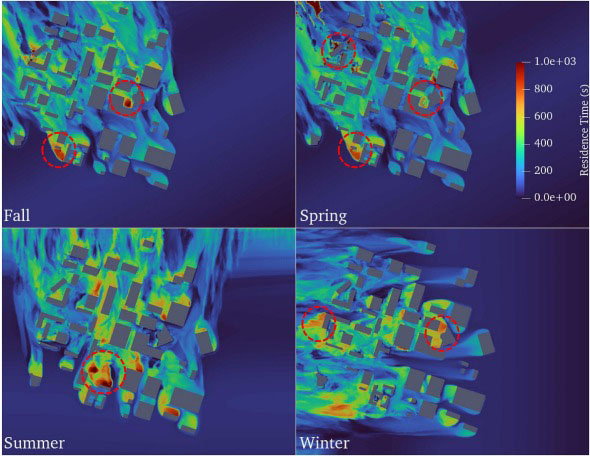
The team modeled the flow of air around buildings at UH. They also used data from a weather station to mimic the wind patterns in 2019.
With this information, they calculated how long it takes for fresh air to replace the existing air in these hot spots, looking at varying conditions such as upward, downward, and forward wind, and studying droplet behavior.
“In our simulations, we studied how the sneeze plume, which is the cloud created by a sneeze, moves in a hot spot. Our findings showed that in certain areas on campus, it can take up to 1000 seconds for fresh air to fully circulate and replace the existing air,” Kia said.
"The findings could inform cleaning protocols, mask policies, and the design of outdoor spaces to minimize disease transmission,” Choi said.
They also found that even a slight upward wind can quickly disperse a sneeze plume close to the ground, but a downward wind can keep the plume in a specific area for a longer time. Additionally, a forward wind can carry the sneeze plume beyond the recommended six feet for social distancing, increasing the risk of infection.
“We also studied the behavior of sneeze droplets and found that most fell to the ground or stuck to surfaces immediately. However, some smaller droplets can remain airborne and travel more than six feet, especially when there is minimal air movement,” Kia said.
The work highlights the importance of adequate ventilation and wind patterns in mitigating transmission of airborne particles and helps in designing more effective strategies for reducing the risk of respiratory disease transmission. This may prompt further research into the role of weather in disease transmission.